|
My Casebook 2015-10-22 Case Report: Amalgam, the only choice that made sense.
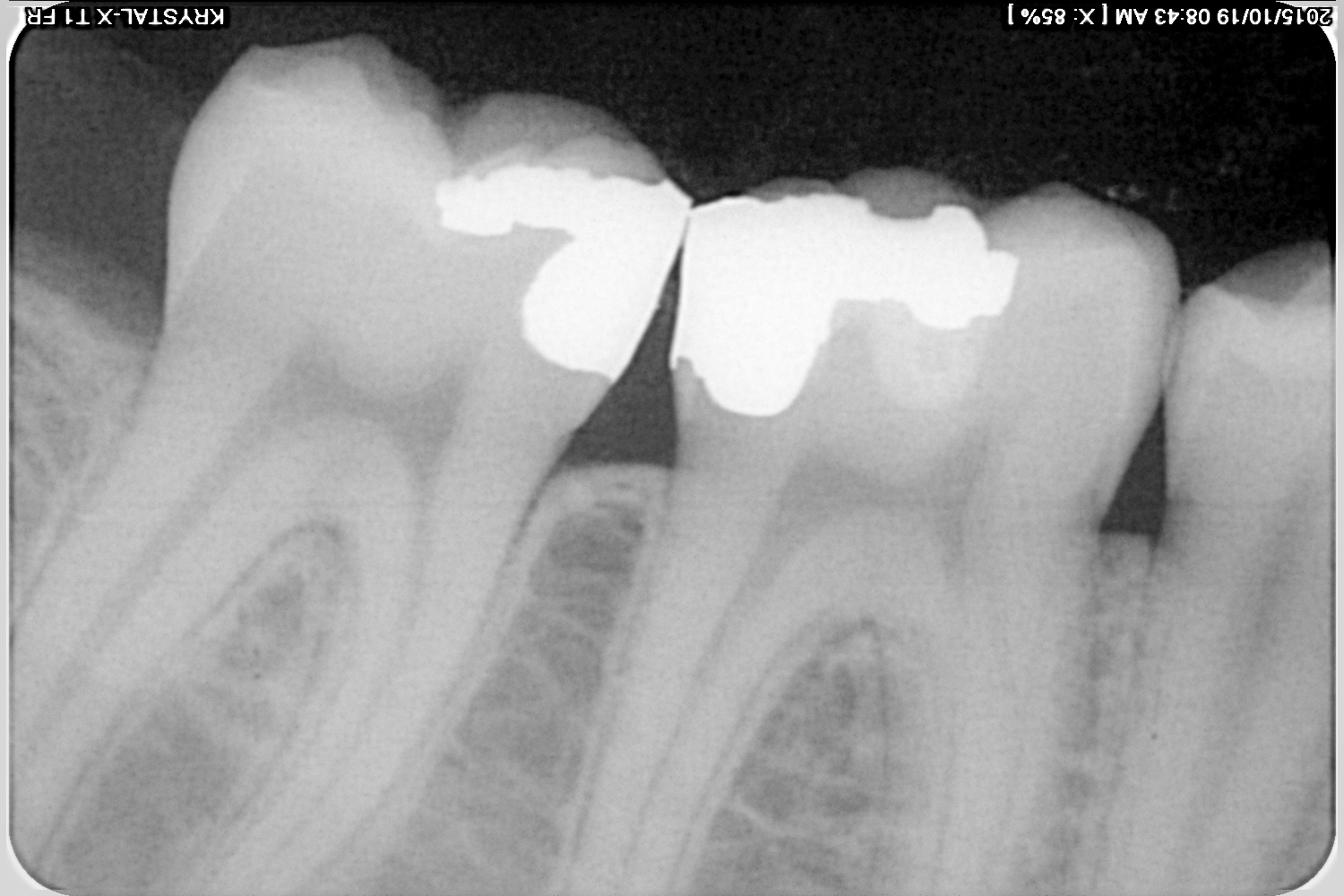
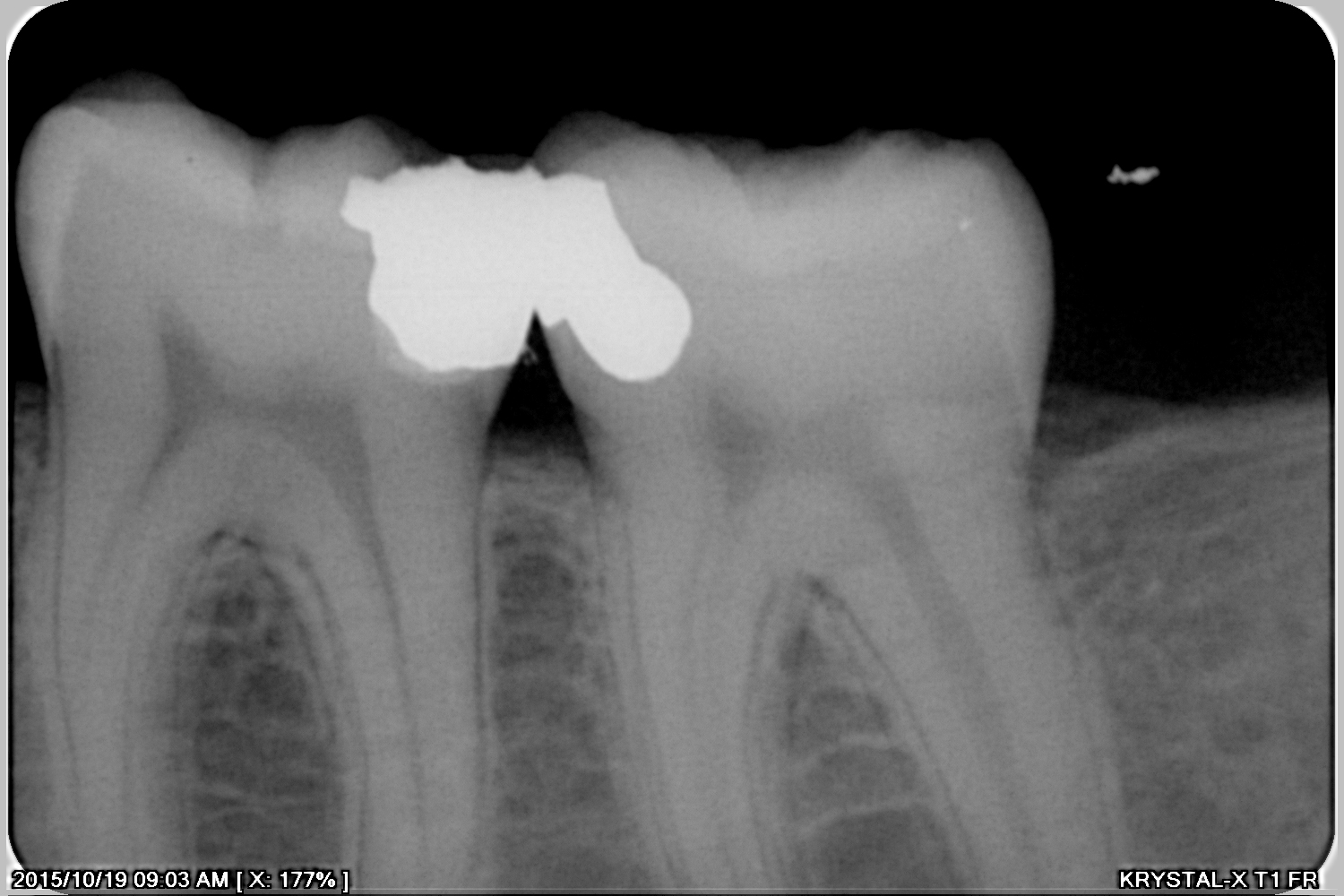
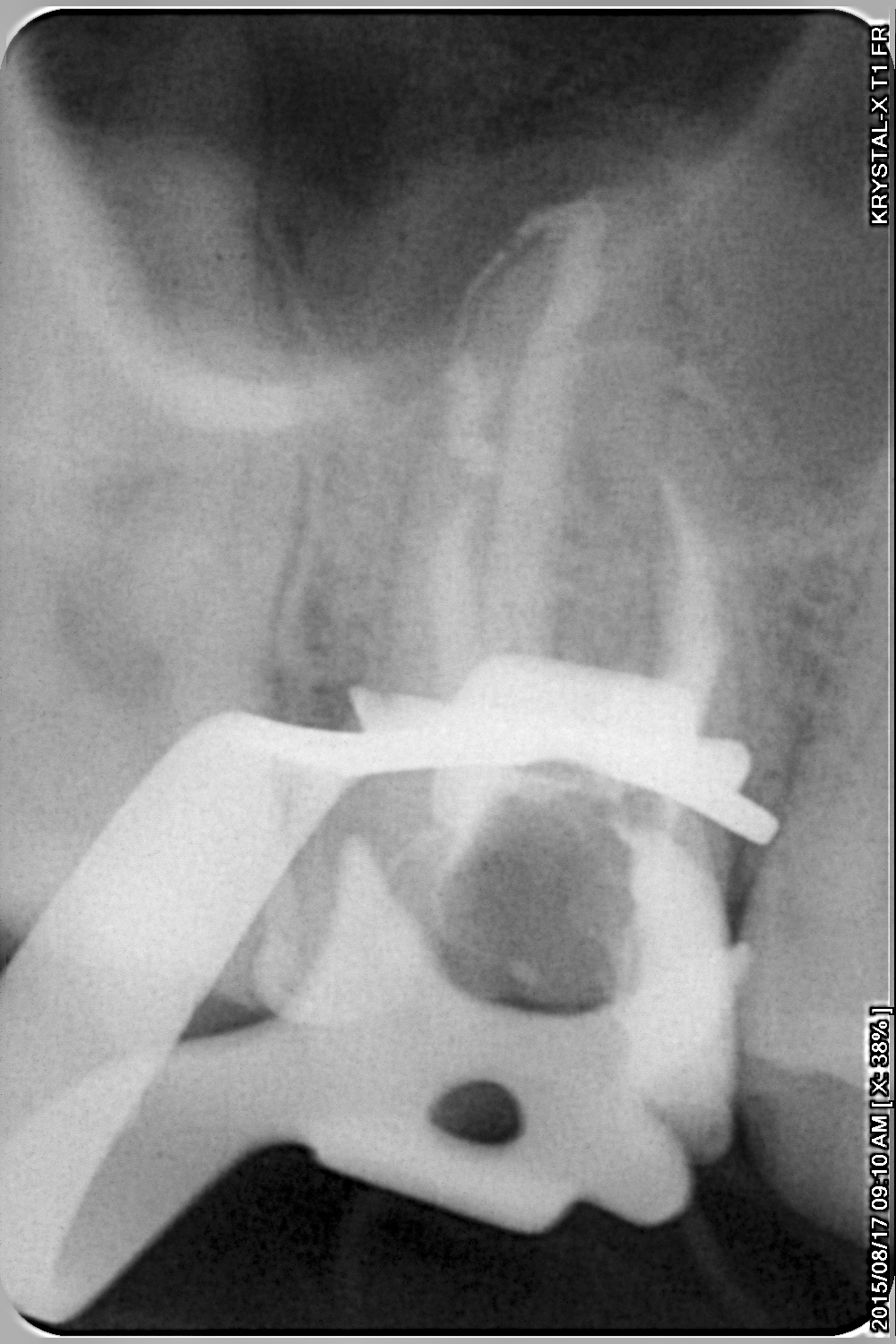
Some professionals claim proudly that they “don’t do amalgam” anymore. Others even propound the untruth that “amalgam is dangerous.” Thirty seven years ago, at university I was told that amalgam restores “only” function, and not esthetics. This may be true, but it is equally true that amalgam is a safe, tried, tested, and the dental profession’s least expensive treatment material. Also, I find it absurd to consider a so-called “esthetic restoration” in an area where I, the dentist find it difficult to actually see the tooth. Why is it necessary to “restore esthetics” in an area that is invisible to the naked eye of the public during normal conversation? I present a case here where the selection of any restorative material other than amalgam would have been fraught with possible side effects and very serious complications. The patient, a 21 year old male student, was referred for the retreatment of the root canal of the 16, (Figure 1). This was confirmed by means of two intra-oral radiographs (Figures 3 and 4). At the outset it was made clear to the patient that not only was he faced with the prospect of a costly retreatment of the root canal of the 16, and subsequent equally costly crown, but there was a real possibility of post-operative sensitivity, pain and discomfort on the other four teeth (36, 37, 46, and 47) requiring even more root canal treatments. There is abundant evidence showing that once enamel has been breached by bacteria, the pulp will be inflamed. As yet there is no definitive way to establish whether this pulpal inflammation will be reversible or irreversible. It is therefore appropriate to always warn a patient presenting with the radiographic views shown in Figures 2, 3 and 4 of the dangers, implications, complications and cost of treatment and alternatives. Now, consider the dangers of placing a leaking restoration on any these four teeth. The physical trauma of the cutting of dentine will exacerbate the inflammation on its own, but to add further insult to injury by placing a restoration that is sealing poorly, will be the final nail in the coffin for the pulp. Now, all bonded restorations, that is “esthetic restorations,” must be placed in a dry working field, and even under the most ideal conditions, there will always be a risk of leakage. The seal of a bonded restoration is at its most optimum, one minute after placement. From that moment onwards, the bond, because of its organic nature, will start to degenerate. Yes, that is the nature of bonded restorations. If you are fortunate you will have an adequate seal after placement, but soon leakage will set in. Nowhere is this more evident than in large direct posterior restorations. Any dentist worthy of the name can testify to the low success rate of large direct posterior restorations. The problem can be circumvented to some extent by using an indirect technique, that is by having a laboratory manufacture the porcelain or resin restoration and then bonding the restoration to the tooth, but it will be a very brave or stupid dentist that will restore all the teeth shown in Figures 2, 3 and 4, that is 36, 37, 46, and 47, with expensive laboratory fabricated restorations, simultaneously. It is impossible to predict what the level of post-operative sensitivity of these teeth will be. It is a very disconcerting moment when a patient returns to the surgery, after having an expensive restoration placed, with a complaint of toothache on said tooth, especially if the only treatment is destruction of the recently placed expensive restoration and root canal treatment. I have long ago decided not to wilfully subject myself to the wrath of these justifiably enraged patients. There is a better way. A freshly placed amalgam leaks. That is why it is advisable to use a cavity varnish before placement. The good news is that from day one, the leakage lessens. Thanks to corrosion, the microscopic gap between tooth and amalgam closes up so that after a few months the amalgam restoration seals perfectly. That is exactly the opposite situation to the bonded restoration that starts to leak as soon as it had been placed. Also, though amalgam should ideally also be placed in a dry working field, as I did with the aid of a rubber dam, it is well known that amalgam is the only material that is relatively immune to moisture contamination. Direct resin restorations and laboratory fabricated restorations have one real advantage over amalgam. They can be placed at the same time without compromising interproximal contact. With amalgam it is impossible to restore the, let us say distal surface of a 36 at the same day as the mesial surface of the 37, as in this case. The dentist’s condensing action of the second restoration will inevitably warp or displace the freshly placed adjacent amalgam surface leading to an open contact. There is only one solution: do the amalgam restorations one at a time, on different days. In this case it would mean four separate visits, if one would not give bilateral inferior alveolar nerve blocks at the same visit. This was exactly the route I took. At first I retreated the root canal of the 16, (Figure 6). This was done over two visits. I then scheduled an appointment to do the crown preparation procedure on this tooth as well as the first visit for the amalgam restorations. On this day I gave the necessary inferior alveolar nerve block, removed the decay on the 46 and 47, placed an amalgam restoration on the mesio-occlusal surfaces of the 47 and an interim restoration consisting of polycarboxylate on the disto-occlusal surfaces of the 46. At the next visit I removed the superficial part of the polycarboxylate interim restoration leaving a deep layer as base and placed the permanent amalgam restoration on the 46 (Figure 7). At two subsequent visits I similarly restored the 36 and 37, one amalgam restoration per visit, again placing a polycarboxylate “temporary dressing” on the 36 at the first visit, and removing the superficial layer and placing amalgam over the polycarboxilate base at the second visit (Figures 8-11). At the sixth and final visit, when I did the 36 amalgam restoration, I also cemented the permanent crown on the 16 (Figure 12), and took post-operative radiographs to confirm the absence of overhangs and quality of fit (Figures 15 and 16). By taking the time and effort to deliberately do the four amalgam restorations, one at a time, that is one per day, I was able to create proper contours which will prevent food impaction. Also, at no stage was any post-operative sensitivity reported. The symptoms of the 16 had also disappeared. I asked the patient whether he was concerned about the dis-esthetics of the “ugly” amalgam restorations to which he responded in the negative, asking me rather incredulously whether I was serious, because he could not even see the restorations. I ran very little risk of post-operative sensitivity, and even if such a complication had arisen on any of the four teeth, the implications would not have been so serious, at least in the patient’s mind’s eye, as would have been the case with expensive porcelain restorations. The amalgam does not rule out the possibility of esthetic restorations at a later stage when enough secondary dentine had been formed and the dentinal tubuli underneath the polycarboxilate had been occluded, minimising the risk of post-operative sensitivity. In this patient’s case I strongly doubt that he would ever request such a service. By taking the cautious route, and the least expensive one, I was able to provide a good service, with the lowest risks of complications. By doing the opposite, the way of “esthetic dentistry,” I would have increased the patient’s financial obligations dramatically, and increased the risk of failure, with concomitant serious financial implications. At the last visit the patient undertook to return within a few weeks, after his university examinations, for the polishing of the amalgam restoration on the 36 which only been placed that day. If I want to be very critical, and we must, I can say that the contour of the distal surface of the 46 is a bit too flat, but I think we can live with that. What I did here was not rocket science. It was common sense, a reflection of Mathew 7:12 “Do unto others…” Why do we see so little of it?
|
| Back | Back to top |
 The panoramic radiograph supplied also showed decay interproximally on the 36, 37, 46, and 47 (Figure 2).
The panoramic radiograph supplied also showed decay interproximally on the 36, 37, 46, and 47 (Figure 2). 

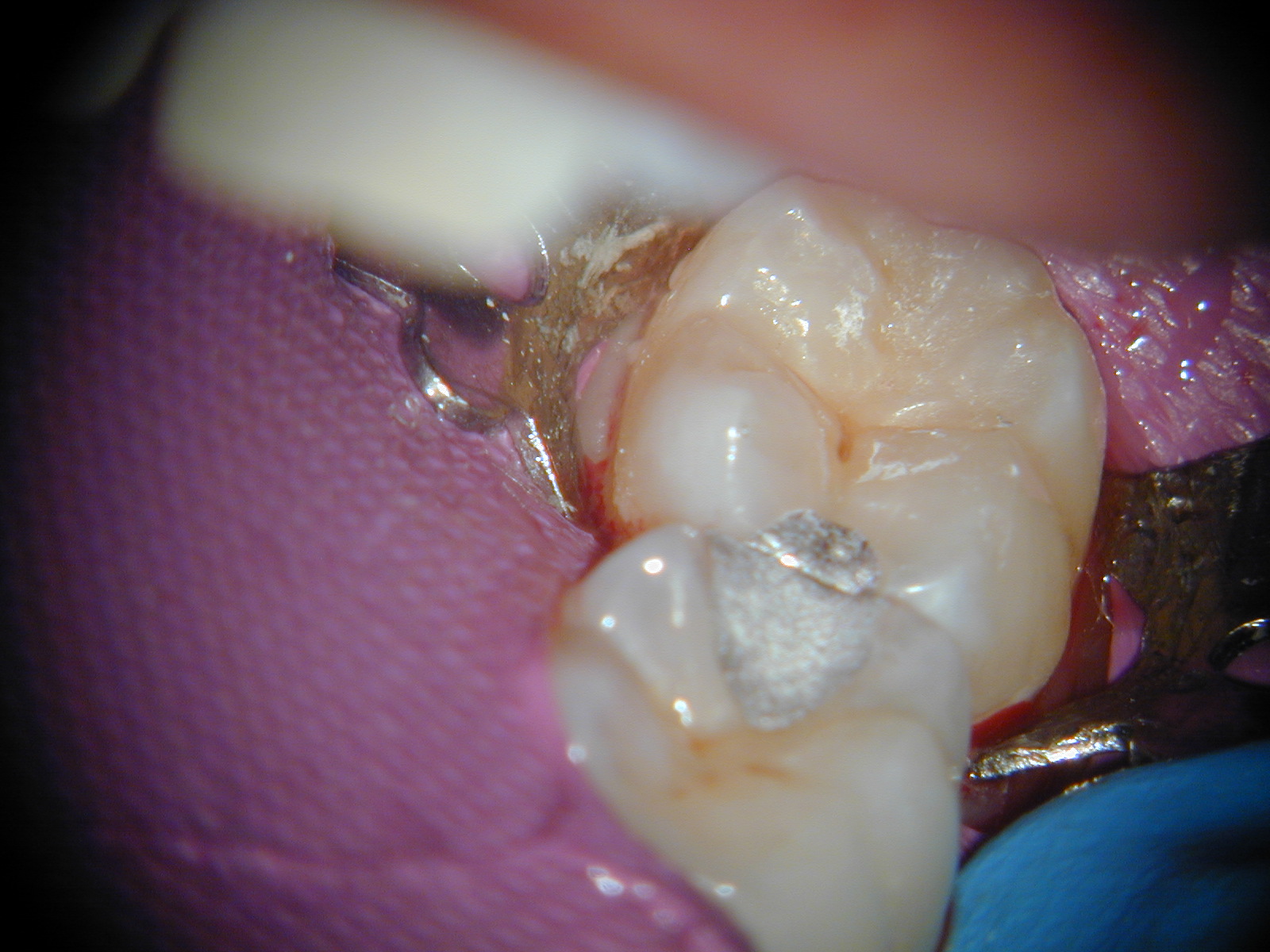
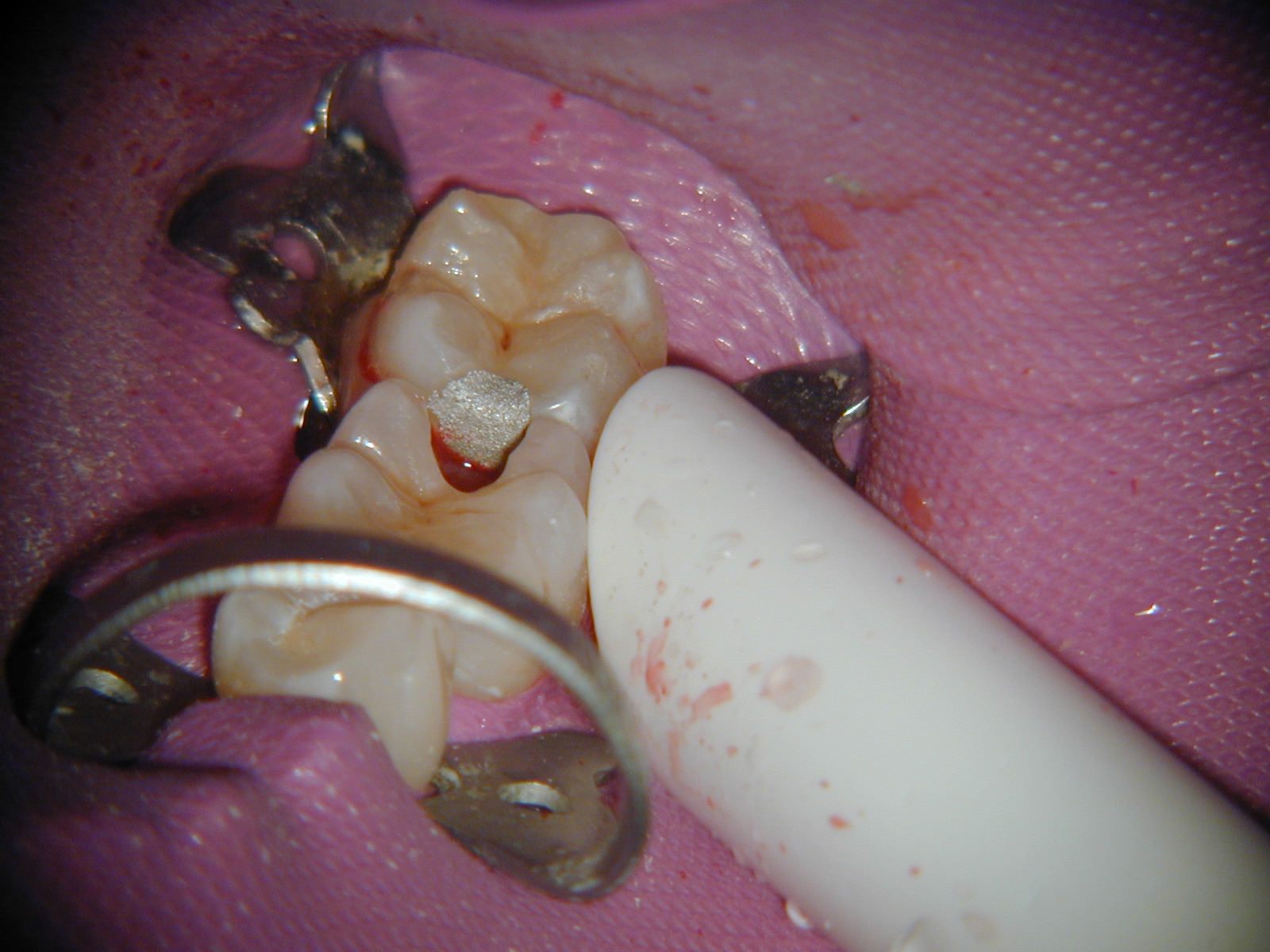
 The pre-operative view of the 36 and 37 is shown in Figure 5. Note that there is no obvious visible external sign of caries.
The pre-operative view of the 36 and 37 is shown in Figure 5. Note that there is no obvious visible external sign of caries.




 polished the three previously placed amalgam restorations (Figures 13 and 14),
polished the three previously placed amalgam restorations (Figures 13 and 14),